Abstract
Introduction
The role of early intensive treatment of multiple myeloma, including tandem autologous stem cell transplantation( ASCT) with bortezomib, thalidomide, dexamethasone( VDT) and melphalan 200mg/m2 as a preparative regimen, followed by 2 years of combination agent maintenance therapy, is being studied. We sought to analyze a cohort of patients who received early intensive treatment at the University of Iowa between 2012 and 2016.
Patients and Methods
All consecutive patients who received early( < 12 months since diagnosis) tandem ASCT and have completed at least 2 years of maintenance therapy between 2012 and 2016 were included for analysis. Planned maintenance therapy consisted of a combination of VDT in 28 day cycles for year 1 and bortezomib, cyclophosphamide and dexamethasone(VCD) in 28 day cycles for year 2. Alternate regimen were used in case of toxicities. The patients were considered to have high risk cytogenetics if they had 17p deletion, t(14;16), amp 1q, or t(4;14) by FISH. Event-free (EFS) and overall survival (OS) probabilities were estimated and plotted using the Kaplan-Meier method. For EFS, time was calculated from date of first transplant to relapse or death due to any cause. Treatment-related mortality was defined as death during transplant phase or maintenance phase due to causes other than disease relapse.The effect of clinical characteristics on outcomes was evaluated using Cox regression models. Estimated effects of predictors are reported as hazard ratios (HR) along with 95% confidence intervals. All statistical testing was two-sided and assessed for significance at the 5% level using SAS v9.4 (SAS Institute, Cary, NC). Responses were measured using IMWG consensus criteria.
Results
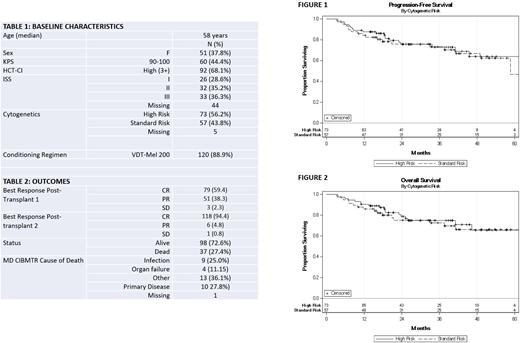
A total of 135 patients met the criteria for inclusion. Key patient characteristics are shown in table 1. The median age at first transplant was 58 years. HCT-CI was high in 68% of patients. 36% of the patients were ISS stage III, and high risk cytogenetics were present in 56%. Preparative regimen was VTD-Mel 200 in 88.9% of patients. Following the first transplant, 59% of patients had achieved CR, and following the second transplant 94.4% of patients achieved CR. At the time of median follow up, 27.4% of patients had died. The cause of death was infection (25%), organ failure (11%), relapsing myeloma (28%) or other (36%).
Univariable analysis identified a statistically significant association only for age with risk of progression or death. Kaplan-Meier curves for progression free survival and overall survival in patients with high risk or low risk cytogenetics are shown in Figures 1 and 2 respectively. The hazard ratio for progression free survival and overall survival in patients with high risk vs low risk cytogenetics was 0.86 (95% confidence interval 0.45 - 1.64, p=0.65), and 0.88 (95% confidence interval 0.45 - 1.73, p=0.71), respectively. The 3 year EFS and OS of patients who received early tandem ASCT followed by 2 years of maintenance were 73% and 72%, respectively.
Following the 2nd autologous transplant, 128 of 135( 94%) patients were started on maintenance therapy. VTD ( 74%) and VRD (6%) were the most common regimens used. Fifty six patients completed maintenance therapy for 1 year without regimen change, and 60 required regimen change due to toxicities. VRD (20), VPomD (9) and VRMp (8) were the most commonly used alternative regimens in the case of toxicities. Following year 1 of maintenance, 96 patients (75%) started a second year of maintenance. VCD (30%) or RD (23%) were the most common regimens. 63(43%) patients completed 2 years of combination maintenance therapy. Grade III-V non-hematologic toxicities during the combined maintenance phase were infection (56%) and peripheral neuropathy (23%) and hematologic toxicities were thrombocytopenia (13%), neutropenia (12%) and anemia (8%).
Conclusion
According to our results, patients with high risk cytogenetics did not have an inferior PFS and OS. These results suggest that in newly diagnosed MM patients, upfront treatment using novel conditioning regimen and tandem ASCT followed by intensive maintenance therapy can result in a very high CR rates, particularly in patients with high risk cytogenetics. Infections and peripheral neuropathies were the most common non-hematologic toxicities during maintenance. Longer follow up will determine further impact of maintenance therapy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal